Posted by George Shaw on Mar 19, 2018
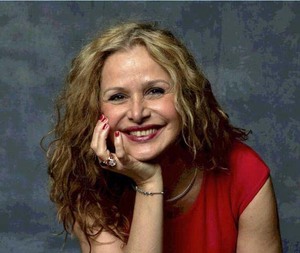
Fabiola Bertinotti attended the ENMC January Summit. She is extensively involved in European FSHD organizations, including being elected in March to a TREAT-NMD patient representative position. Fabiola also attended this year's Annual Auction in January, at which her son Jaya addressed the attendees.
From Passive to Active!
ENMC Summit “The Patient Role in Shared Decision Making”
by Fabiola Maria Bertinotti
January 31, 2018
I was recently among the many representatives in the world of neuromuscular diseases invited to the European NeuroMuscular Centre (ENMC) meeting held in Milan on January 19-20. I was more than honored to sit amongst this group of talented professionals in my capacity of Head of Family’s Interests for FSHD EUROPE, a federation of local patient associations in the field of Facioscapulohumeral Muscular Dystrophy (FSHD) and other MD’s, and additionally as a representative for Coordination Of Neuromuscular Associations, Italy (CAMN).
I must say that I felt in general particularly excited with this workshop, and I imagine most everyone else attending felt the same. We were all very conscious that this 235th ENMC workshop marked the marked the 25th anniversary for ENMC, an international organization whose specialty has been organizing meetings on the most valuable trends in the neuromuscular space by pulling together the most significant personalities of a given field in order to raise the bar on a variety of compelling topics. Strictly tied to the importance of this anniversary was the theme of the meeting, “The position of the neuromuscular patient in Shared Decision Making”.
Although Shared Decision Making (SDM) applies to all key stakeholders involved with the patient/doctor relationship, it was clear from the beginning that the main purpose of this workshop was that of redefining the role of patients over the next 10 years to that of a decision-maker. This large step forward in the world of medicine and science will have at least two key substantial consequences:
- The patient will be seen as an individual enabled to participate in medical decisions impacting his/her health.
- The patient who wishes to become knowledgeable will be acting as an expert of his/her own disease and also will be taking an increasingly decisive role in the success of scientific trials, other patients' awareness and formation initiatives, relations with the pharmaceutical industry and public health institutions.
The European Community has been on the front line, supporting this new patient role over the past 2-3 years, mainly through the creation of high-end organizations such as EURORDIS and EUPATI. The former being a non-governmental patient-driven alliance of patient organizations representing 779 rare disease patient organizations in 69 countries, and the latter the European Patients’ Academy, a pan-European project implemented as a public-private partnership by a collaborative multi-stakeholder consortium from the pharmaceutical industry, academia, not-for-profit, and patient organizations.
In the past, the role of patients in the design of clinical trials was absent, which may be one of the factors why these trials did not meet either the patient’s or the regulatory requirements. This is why I was extremely pleased with the ENMC highlighting this very crucial issue, showing a willingness to play a frontline role by addressing the issue of patient participation in a broader manner, covering multiple research aspects, and inviting patients representing several areas of disease. In fact, the ENMC itself has had a patient participation program in place for 4 years. There have always been at least 2-3 patients and/or patient representatives invited to each workshop, where they play an active role and influence the setting of priorities in the research agenda.
Many topics related to the patient role in SDM were thoroughly debated during this ENMC meeting, and two different breakout sessions saw passionate participation of all participants around 6 main themes:
- research that has a major impact on day-to-day patient life
- psychosocial support at screenings and diagnosis
- transition from childhood to adulthood
- disease registries and biobanks
- clinical trial design
- regulatory aspects
The output of these intense two days, composed of lectures and discussion groups, was collected by three editors who will write a draft article that will be revised later on by participants, with the final goal of becoming a publication in key scientific magazines in six months' time. That said, as the mother of a patient living with FSHD, these are my take-away items:
- Shared Decision Making is a process, and as such, it requires a change in approach and a culture shift by all stakeholders, as well as more financial support, societal integration and contemporary services.
- Everyone needs to be educated on the benefits of SDM, from physicians, to healthcare practitioners, to caregivers, and especially to both the younger and adult patients themselves.
- Structural changes are needed in order to include Patient Organizations (PO’s) and Patient Representatives (PR’s) in advisory boards, ethics committees, and in every stage of clinical trials.
- Patients who feel able to, should become ambassadors, inspiring other patients as well, and becoming constructive partners with all stakeholders involved.
- Like everywhere, honesty and transparency are crucial.
- Continuous financial support from the European Union and local public administrations is essential in order to both make SDM happen and sustain it.
- Fluid and respectful communication amongst all stakeholders is a must, and patients should sit at the top level of the “participation ladder”.
- Independence is a key factor in ensuring a successful balance of all parties involved.
- The circular flow of information is fundamental in clinical trial design, protocol, recruiting, patient-reported outcomes, and outcomes measures. SDM is a process that is going to be successful only if all stakeholders work together.
- SDM can definitely play a significant role also in registries and biobanks.
- Each of the local neuromuscular disease registries must normalize its data and in general be structured in a way as to permit international linkage to other registries, as they exist for the benefit of patients in the first place.
- Patients need to be informed so that they can take part on the process.
- The decision of patients must be respected, whether or not they are willing and ready to become experts.
- Coaching and Awareness are the first steps in initiating SDM, so the human factor is key when focusing on the patient as a key player in a scientific/clinical paradigm.
- Advocacy should be offered through videos, info graphics, etc., to patients in order to place them in a position to make decisions.
- Patients should be continually informed about the evolution of the registries, and receive feedback about the use of their samples and/or data. This will encourage their involvement and make them feel part of the research and therefore their own future!
- Key clinicians in the space of FSHD, like Dr. Georg Padberg (ENMC’s Research Director) and Baziel Van Engelen, were attending, hence FSHD community is in a good position to embrace a more contemporary approach, at least from the side of two key clinicians!
- Last but not least, patients’ reps, clinicians and pharmaceutical reps were all present. European countries were largely represented. The organization of the meeting was definitely very good across the board. I am looking forward to seeing all of this content orderly laid out in a comprehensive article which - I hope - will lead the way to what is called “co-creation” and “open science”.




Connect with us on social media